eNews is a monthly e-newsletter shared with the global PEN Community and created to help dietitians position themselves as leaders in evidence-based nutrition practice. In addition, users of the PEN System will find articles on the new evidence, resources and features available and how to maximize one's use of PEN.
PEN® TEAM and FRIENDS’ SURPRISING FINDINGS OF 2017
PEN® Surprising Finding: Nutritional Implication of Legalizing Cannabis
PEN® Surprising Finding: Migraine Headache Triggers
PEN® Surprising Finding: Are Avocados Really That Good?
PEN® Surprising Finding: Nudge Theory
PEN® Surprising Finding: Who is King - Casein or Whey Powder?
PEN® Surprising Finding: Healthy Diets Costs Households 15 Per Cent Less Than Current (Unhealthy) Diets
PEN® Surprising Finding: B Vitamins
PEN® Surprising Finding: Using Eye-Tracking Technology to Assess Consumer Shopping Behaviour
PEN® Surprising Finding: Plant-based Beverages and Young Children
PEN® Surprising Finding: Migraines and Protein Recommendations for Vegetarian Athletes
PEN® Surprising Finding: It Just Makes You Smile
PEN® Surprising Finding: The Appendix – A Good Bacteria Storehouse
PEN® Surprising Finding: Gut Microbiome
PEN® Surprising Finding: Mouth Rinsing and Sports Performance
PEN® Surprising Finding: Sweating Blood and Artificial Intelligence
PEN® Surprising Finding: Non-celiac Gluten Sensitivity (NCGS) and Gluten Restriction
PEN® Surprising Finding: Nutritional Implication of Legalizing Cannabis
Are there nutritional implications of the legalization of the recreational use of cannabis (marijuana) in Canada or elsewhere?

Cannabis has been legal for medicinal use in Canada since 2001 (1). With the prospect of it being legalized for recreational use in July 2018, I wanted to see if there are any nutritional implications the PEN
® Team should be publishing. The main area of concern by Canadians is the impact legalization might have on the developing brains of children and youth.
The primary medical use, based on limited evidence, of cannabis and cannabinoids has been for chronic non-cancer pain control, e.g. multiple sclerosis, anorexia in HIV and nausea and vomiting in people undergoing cancer treatment (2). More recently it has been used for anxiety, spasticity, fibromyalgia and epilepsy. Some early stage research is also looking at its use in rheumatoid arthritis and inflammatory bowel disease. Contraindications for use are those with psychosis, schizophrenia, unstable heart disease and who are pregnant. There are two strains: Indica, which is a sedative, and Sativa, which is a stimulant. It is suggested that medical cannabis is best used under the supervision of an experienced health care professional.
I was surprised that while there was no research related to any nutrient interaction found, there were several articles of interest concerning toxicity and the possibility of it triggering a food allergy. With the legalization of recreational use, it is predicted that we will see cannabis and its principal active constituent, Δ9-tetrahydrocannabinol (THC) used in an increasing number of edible products (3). Cases of toxicity have been noted as adults and children unknowingly consume products made with cannabis. Therefore, it is recommended that there needs to be an increase in general public awareness regarding the potential hazards of THC-containing edibles that resemble commercially available food products.
Finally, another aspect to be aware of is the potential for crossed allergy with food or cannabis-fruit-vegetable syndrome (4). As the use of cannabis has increased, cannabis allergies, including contact allergies, have increased from a simple runny nose to anaphylactic-type reactions. Cannabis contains lipid transfer proteins (LTP) called Can s 3. LTPs are present in many vegetables and fruit and they have a similar chemical structure leading to incidences of cross-allergies with foods. The main food allergies seen by this cross-allergy are: bananas, grapes, peanuts, hazelnuts, other nuts, apples, peaches, cherries, wheat, barley and citrus fruits. Tomatoes and spinach may also be cross-allergens but have not been seen as frequently as the preceding list. A non-food cross-allergy may also be seen with latex. There has also been a reported case of an eight-year-old child who developed some of these cross-food allergies from passive smoke from a parent smoking cannabis around the child.
Implications for Practice: Practitioners should be aware of the cannabis-containing food products that are and will be on the market. Many of them, such as cakes, cookies and candies, are probably not viewed as part of a healthy diet. Also, when a client presents with newly acquired food allergies one might screen for cannabis use - either smoking or ingestion.
References
- University of Alberta. Cannabis use in Canada | By the numbers (cited 2017 Nov 24). Available from: https://www.ualberta.ca/public-health/about/this-is-public-health/what-is-public-health/cannabis-use-in-canada
- Katz D, Katz I, Porat-Katz BS, Shoenfeld Y. Medical cannabis: another piece in the mosaic of autoimmunity? Clin Pharmacol Ther. 2017 Feb;101(2):230-8. doi: 10.1002/cpt.568. Epub 2016 Dec 20. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/27859024
- Vo KT, Horng H, Li K, Ho RY. Wu AHB, Lynch KL, Smollin CG. Cannabis intoxication case series: the dangers of edibles containing tetrahydrocannabinol. Ann Emerg Med. 2017 Nov 3. pii: S0196-0644(17)31657-8. doi: 10.1016/j.annemergmed.2017.09.008. [Epub ahead of print]. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/29103798
- Drouet M, Hoppe A, Moreau AS, Bonneau JC, Leclere JM, Le Sellin JP. Cannabis et allergie croisée alimentaire, [Cannabis and crossed allergy with food]. [Article in French]. Rev Pneumol Clin. 2017 Nov 6. pii: S0761-8417(17)30120-7. doi: 10.1016/j.pneumo.2017.09.003. [Epub ahead of print]. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/29122396
Written by:
Beth Armour, MEd, P.Dt
PEN
® Content Manager
Dietitians of Canada
PEN® Surprising Finding: Migraine Headache Triggers
As someone who suffers from migraine, I am always on the lookout for help in reducing the number and severity of migraines that I get. In the past few years, newer research has resulted in substantial changes to the list of potential

dietary triggers (1). No longer on the list are some old standbys such as chocolate, tyramine and MSG. Several others triggers, such as alcohol, caffeine consumption and dehydration, have been identified by sufferers as triggers, but the evidence for them is conflicting and inconclusive. Because triggers differ between individuals, and sometimes between migraine episodes, individuals who suffer from migraines should still be encouraged to experiment to identify their own triggers, including other potential environmental factors. For additional information and tools and resources see: the
PEN Nervous System - Migraine Knowledge Pathway.
References
- Dietitians of Canada. What dietary components, if any, are triggers for migraine among adults and children who suffer from migraines? In: Practice-Based Evidence in Nutrition [PEN]. 2017 August 9 [cited 2017 Nov 1]. Available from: http://www.pennutrition.com/KnowledgePathway.aspx?kpid=11148&pqcatid=146&pqid=9068. Access only by subscription.
Written by:
Kerri Staden, BSc, RD
PEN
® Resource Manager
Dietitians of Canada
PEN® Surprising Finding: Are Avocados Really That Good?
Advertisements are promoting avocados as the only recommendable source of fat. A highly cited avocado study (1) has a weakness that makes their conclusions invalid and worth looking at in more depth.
.jpg)
The study compared carotenoid (lutein, beta-carotene, alpha-carotene, lycopene) absorption between meals. The control meals were designed to be low in fat: 1) 300 grams of salsa with three slices of bread, both fat-free, and 2) 220 grams of salad (carrots, lettuce, spinach) with fat-free salad dressing and two slices of fat-free bread. The test meals were the same with the addition of 75 and/or 150 grams of avocado or 24 grams of avocado oil. The study found that the additions of avocado or avocado oil increased the absorption of the carotenoids.
The study concluded: “In conclusion, adding avocado fruit can significantly enhance carotenoid absorption from salad and salsa, which is attributed primarily to the lipids present in avocado”. This study was funded by The California Avocado Commission.
Advertisements have attributed these findings to avocado, while this absorption facilitation effect is not a unique property of these fruit. Other studies reveal that the absorption of carotenoids (as well as other fat-soluble vitamins (2)) are improved by adding oils, in a dose-response manner (2,3).
Avocados are highly perishable and an expensive source of fat, which some people may not be able to afford as a regular and important fat source. Most people need information about other sources of fats with desirable fatty acids ratios, such as canola, soy and olive oils.
References
- Unlu NZ, Bohn T, Clinton SK, Schwartz SJ. Carotenoid absorption from salad and salsa by humans is enhanced by the addition of avocado or avocado oil. J Nutr. 2005;135(3):431-6. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/15735074
- White WS, Zhou Y, Crane A, Dixon P, Quadt F, Flendrig LM. Modeling the dose effects of soybean oil in salad dressing on carotenoid and fat-soluble vitamin bioavailability in salad vegetables. Am J Clin Nutr. 2017 Oct;106(4):1041-51. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/28814399
- Goltz SR, Campbell WW, Chitchumroonchokchai C, Failla ML, Ferruzzi MG. Meal triacylglycerol profile modulates postprandial absorption of carotenoids in humans. Mol Nutr Food Res. 2012 Jun;56(6):866-77. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/22707262
Written by:
Tanis Fenton PhD RD FDC
Dietitian/Nutritionist, Epidemiologist,
PEN
® Evidence Analyst Associate Professor, University of Calgary
PEN® Surprising Finding: Nudge Theory
While looking through the BDA’s publication
Dietetics Today, I was interested to read the article on page 18:
Fast Facts by Jennifer Low, a lead dietitian for a bariatric service. Jennifer said, “research has found that intentional nudges led to a 15% increase in

healthier nutrition choices”. Intrigued I looked up the systematic review by Arno and Thomas (1). The authors identified an initial 5,436 studies, reduced to 42 through screening and applying their inclusion criteria, which included being about the general population (not aimed at a specific group e.g. people with diabetes) and aimed at “influencing behaviour related to food consumption”. The influencing had to be done by altering what is known as “choice architecture”, which included the placement of foods either on a supermarket shelve or in a menu, their labelling and their portion size. Outcomes were either purchases measured via receipts or energy content. The authors reported that the majority of included studies came from the U.S., with 31% of the sample sizes between 100 and 500 subjects, but the majority having less than 100 subjects. The meta-analysis showed, as Jennifer had quoted, an average 15% increase in healthier choices.
Some of the nudges employed were simply to offer less healthy snacks in smaller portions or at a greater distance away from the consumer and make healthier food available more easily and in larger portions. Techniques we dietitians have been employing for years, such as when my children were young the fruit bowl lived on top of the television while biscuits and crisps were hidden in kitchen cupboards. Maybe the surprise is not the findings, but that supermarkets and restaurants are slowly being persuaded to use nudge theory to sell healthier products. I must go and search PubMed for a review and see if that is indeed the case and if so what proportion of retailers are actively using nudge theory.
References
- Arno A, Thomas S. The efficacy of nudge theory strategies in influencing adult dietary behaviour: a systematic review and meta-analysis. BMC Public Health. 2016 Jul 30;16:676. doi: 10.1186/s12889-016-3272-x. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/27475752.
Written by
Judy Lawrence, RD, PhD
PEN
® Evidence Analyst
Research Officer
British Dietetic Association
PEN® Surprising Finding: Who is King - Casein or Whey Powder?
One of the more interesting findings from my research and writing over the past year had to do with casein protein for supporting muscle protein synthesis rates (MPS). Whey protein has always worn the crown of “best” or “better” as having  “the advantage” over all other supplemental proteins (1). This is due to its rapid digestion and absorption and its higher leucine content; the latter of which helps stimulate MPS. Casein, particularly micellar casein, is slower to digest and absorb. Casein hydrolysates are faster; however, because they are hydrolyzed. However, whey may have also been deemed better because of how short the studies were that evaluated MPS rates. Most studies comparing whey to casein did not study MPS rates long enough to allow casein to showcase its talents. Research that observed subjects for up to six hours after resistance exercise and protein ingestion found no difference between whey and casein over the full six-hour period; although there were differences in the early versus late periods. Hence, over 12-24 hours, these two proteins may be equivalent for helping augment MPS rates. Additionally, longer term research (months versus hours) reported no differences between whey and casein for muscle hypertrophy over a resistance-training program.
“the advantage” over all other supplemental proteins (1). This is due to its rapid digestion and absorption and its higher leucine content; the latter of which helps stimulate MPS. Casein, particularly micellar casein, is slower to digest and absorb. Casein hydrolysates are faster; however, because they are hydrolyzed. However, whey may have also been deemed better because of how short the studies were that evaluated MPS rates. Most studies comparing whey to casein did not study MPS rates long enough to allow casein to showcase its talents. Research that observed subjects for up to six hours after resistance exercise and protein ingestion found no difference between whey and casein over the full six-hour period; although there were differences in the early versus late periods. Hence, over 12-24 hours, these two proteins may be equivalent for helping augment MPS rates. Additionally, longer term research (months versus hours) reported no differences between whey and casein for muscle hypertrophy over a resistance-training program.
It was the above findings, combined with hearing anecdotal reports of body builders stating they prefer casein over whey and that many like to take casein before bed, that got me to take another look into PubMed where I found an interesting review on pre-sleep protein nutrition combined with resistance exercise for muscle protein synthesis (2). After observing that MPS rates overnight tended to be low, even in those who ate enough protein over the day, the review authors hypothesized that if amino acids were available overnight that MPS rates could be even further enhanced.
In feeding 30-40 g of casein protein before bed (a few hours after resistance exercise) and taking blood and biopsies over the night, authors found that the protein was digested and absorbed well, amino acids appeared in the blood, MPS rates were elevated, muscle protein breakdown was lessened, and the tracers in the casein were incorporated into de novo myofibrillar protein synthesis. The authors recommend casein over whey for pre-sleep protein feeding due to the sleeping period being typically six to eight hours and the slower digestion and absorption of casein over whey. However, a head to head comparison of the different protein types for pre-sleep remains to be done. Authors stated that a variety of animal proteins from chicken to eggs to steak to yogurt could accomplish this augmentation in MPS rates over night.
How this practice may impact long-term training adaptations to resistance exercise, other exercise modalities, and even clinical situations to offset muscle loss in the bedridden will be an exciting area of research to keep an eye on. Studies that have evaluated the effects of protein timing have rarely controlled overall daily dose while manipulating timing. In other words, investigators tended to give placebo or protein at a set time in relation to the exercise or in relation to sleep, compare the effects in the two groups and attribute findings to timing. However, unless there is another control group also getting the same total amount of protein as the experimental group, over the period of a full day (24 hours) than it cannot be said with certainty that the observed effects are due to timing alone; even though MPS was elevated acutely. Acute changes in MPS (hours) have not always perfectly predicted changes in mass and strength over longer time periods (months).
Regardless, the authors felt that the overnight period is an additional opportunity to intervene and shift the balance away from muscle protein breakdown and towards muscle protein synthesis.
References
- Dietitians of Canada. What is the optimal amount, type and timing of protein intakes for athletes? In: Practice-Based Evidence in Nutrition [PEN]. 2017 October 19 [cited 2017 Nov 1]. Available from: http://www.pennutrition.com/KnowledgePathway.aspx?kpid=8180&pqcatid=146&pqid=11977. Access only by subscription.
- Trommelen J, Kouw IWK, Holwerda AM, Snijders T, Halson SL, Rollo I, et al. Pre-sleep dietary protein-derived amino acids are incorporated in myofibrillar protein during post-exercise overnight recovery. Am J Physiol Endocrinol Metab. 2017 May 23:ajpendo.00273.2016. doi: 10.1152/ajpendo.00273.2016. [Epub ahead of print]. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/28536184
Written by:
Heather Petrie, MSc, RD
PEN® Evidence Analyst
Dietitians of Canada
PEN® Surprising Finding: Healthy Diets Costs Households 15 Per Cent Less Than Current (Unhealthy) Diets
Each year, I have the privilege of being able to look over in advance the abstracts of the research being presented at the DAA National Conference, so that I can prepare media communications to profile some of this exciting work.
As I went through this process earlier in the year, one paper really struck a chord with me. It described research by .jpg) Professor Amanda Lee, one of the plenary presenters at the conference.
Professor Amanda Lee, one of the plenary presenters at the conference.
Professor Lee’s research found that, contrary to public perception, healthy diets are more affordable than current (unhealthy) diets – and in fact, they cost Australian households 15 per cent less (1).
Her findings highlighted that Australian households spend the majority (58%) of their food budget on discretionary or ‘junk’ foods and drinks, including take-aways (14%) and sugar-sweetened beverages (4%). Australian Health Survey data shows that few Australians consume diets consistent with national recommendations.
Professor Lee commented that less than four per cent of Australians eat adequate quantities of healthy foods, yet more than 35 per cent of energy (kilojoule) intake comes from discretionary foods and drinks, which provide little nutrition – and this is hurting the health (and the hip pocket) of many Australians.
Her research also found that, although healthy diets cost less than current (unhealthy) diets, people in low income households need to spend around a third (31%) of their disposable income to eat a healthy diet, so food insecurity is a real problem in these households.
Through her plenary presentation at the conference, Professor Lee stressed that Australia needs a coordinated approach to nutrition policy, and she called on the Australian Government to update, fund and implement a new National Nutrition Policy, as the current policy was developed 25 years ago.
References
- Lee AJ, Kane S, Ramsey R, Good E, Dick M. Testing the price and affordability of healthy and current (unhealthy) diets and the potential impacts of policy change in Australia. BMC Public Health 2016; 16: 1-22. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/27067642
Written by:
Maree Hall, MND, APD
Senior Public Relations Manager
Dietitians Association of Australia
PEN® Surprising Finding: B Vitamins
I recently had a physician ask me if there was robust evidence to support the claim sometimes made about vitamin B12 improving “energy”. I turned to the Office of Dietary Supplements (National Institutes of Health) vitamin B12 fact sheet and .jpg) noted that vitamin B12 is often promoted as an “energy enhancer”. This is probably because of its role as a coenzyme in metabolic pathways and if you have a deficiency of vitamin B12, it can cause megaloblastic anemia, which is associated with fatigue and weakness. When vitamin B12 deficiency is treated with vitamin B12, the symptoms improve. However, there is no evidence that healthy individuals with normal vitamin B12 levels will experience enhanced energy by taking vitamin B12 supplements.
noted that vitamin B12 is often promoted as an “energy enhancer”. This is probably because of its role as a coenzyme in metabolic pathways and if you have a deficiency of vitamin B12, it can cause megaloblastic anemia, which is associated with fatigue and weakness. When vitamin B12 deficiency is treated with vitamin B12, the symptoms improve. However, there is no evidence that healthy individuals with normal vitamin B12 levels will experience enhanced energy by taking vitamin B12 supplements.
I noted that the Recommended Dietary Allowance for vitamin B12 is 2.4 micrograms for adults and that the Institute of Medicine did not establish an upper level (UL) for vitamin B12, stating that: “no adverse effects have been associated with excess vitamin B12 intake from food and supplements in healthy individuals” (1).
So, I was surprised to see the recent article by Brasky, et al. suggesting an association between long-term use of supplemental B vitamins and increased lung cancer risk (2). The authors used data collected from the VITAL cohort (3), a prospective cohort of more than 77,000 individuals living in the U.S., which is designed to examine long-term use of supplements and any relationship to cancer. They controlled for a number of relevant confounding variables that might explain or impact on the findings.
Specifically, they found that when they examined the average supplement dose over 10 years, there was almost a doubling of the risk of lung cancer in the group of men taking the highest amounts of vitamins B6 and B12:
- vitamin B6 intakes of 20 mg/day: hazard ratio 1.82; 95%CI, 1.25 to 2.65
- vitamin B12 intakes of 550 ug/day: hazard ratio 1.98; 95%CI, 1.3 to 2.97.
The risk was higher still in men who smoked. They did not find any association between vitamins B6, folate, and B12 and cancer risk in women. The relationship applied to several kinds of lung cancer, but not adenocarcinoma.
Implications for Practice: This is an observational study so it does not prove that high doses of vitamins B6 and B12 cause cancer. The authors did not address the situation of individuals taking long-term vitamin B12 supplements due to a lack of intrinsic factor. However, these findings suggest that individuals should not be advised to consume large doses of supplemental vitamin B6 or B12 to prevent cancer as it may increase the risk of lung cancer in men and especially in those who smoke.
References
- Institute of Medicine. Dietary Reference Intakes: thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline. Washington, DC: National Academy of Sciences; 1998 p 346. Available from: https://www.ncbi.nlm.nih.gov/books/NBK114310/
- Brasky TM, White E, Chen CL. Long-term, supplemental, one-carbon metabolism-related vitamin B use in relation to lung cancer risk in the vitamins and lifestyle (VITAL) cohort. J Clin Oncol. 2017 Oct 20;35(30):3440-8. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/28829668
- White E, Patterson RE, Kristal AR, Thornquist M, King I, Shattuck AL, et al: VITamins And Lifestyle cohort study: study design and characteristics of supplement users. Am J Epidemio. 2004 Jan 1;159(1):83-93. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/14693663
Written by Jayne Thirsk, RD, PhD, FDC
Director, PEN
®
Dietitians of Canada
PEN® Surprising Finding: Using Eye-Tracking Technology to Assess Consumer Shopping Behaviour
I was pleasantly surprised to learn about some exciting food retail research coming from the University of Guelph Longo's Food Retail Lab. Using eye-tracking and camera technology researchers will study what matters to shoppers while they browse the lab’s mock grocery aisles and assess their decision-making when purchasing foods. This will provide many opportunities for students to be involved in research along with providing some interesting information that health, policy, marketing and other stakeholders can use in their practices. The four initial research priorities are:
Longo's Food Retail Lab. Using eye-tracking and camera technology researchers will study what matters to shoppers while they browse the lab’s mock grocery aisles and assess their decision-making when purchasing foods. This will provide many opportunities for students to be involved in research along with providing some interesting information that health, policy, marketing and other stakeholders can use in their practices. The four initial research priorities are:
identifying how people make pricing decisions, considering brands, packages sizes and unit pricing
the effect of food labelling (e.g. genetically modified organisms (GMO)-free), on product choice
how much or how little people read and process food packaging information
how nutritional labelling information on grocery shelves influences choice. For more information on the Guelph Longo's Food Retail Lab see:
https://www.uoguelph.ca/business/food-innovation-research-lab
https://news.uoguelph.ca/2017/05/high-tech-food-labs-aim-understand-consumer-needs/
For more information see:
Food and Nutrition Labelling Knowledge Pathway.
Written by:
Jane Bellman, MEd, RD
PEN
® Resource Manager
Dietitians of Canada
PEN® Surprising Finding: Plant-based Beverages and Young Children
For me, the article, Trending Topics: Plant-based Beverages - Are They Really Healthier for Young Children? (1), was a 'simple' matter of pointing out some existing information and packaging it in a way that drew my attention to it. Scientific information is
of no practical use if we don't take the time to digest its meaning and incorporate its significance into our practice in a proactive manner.
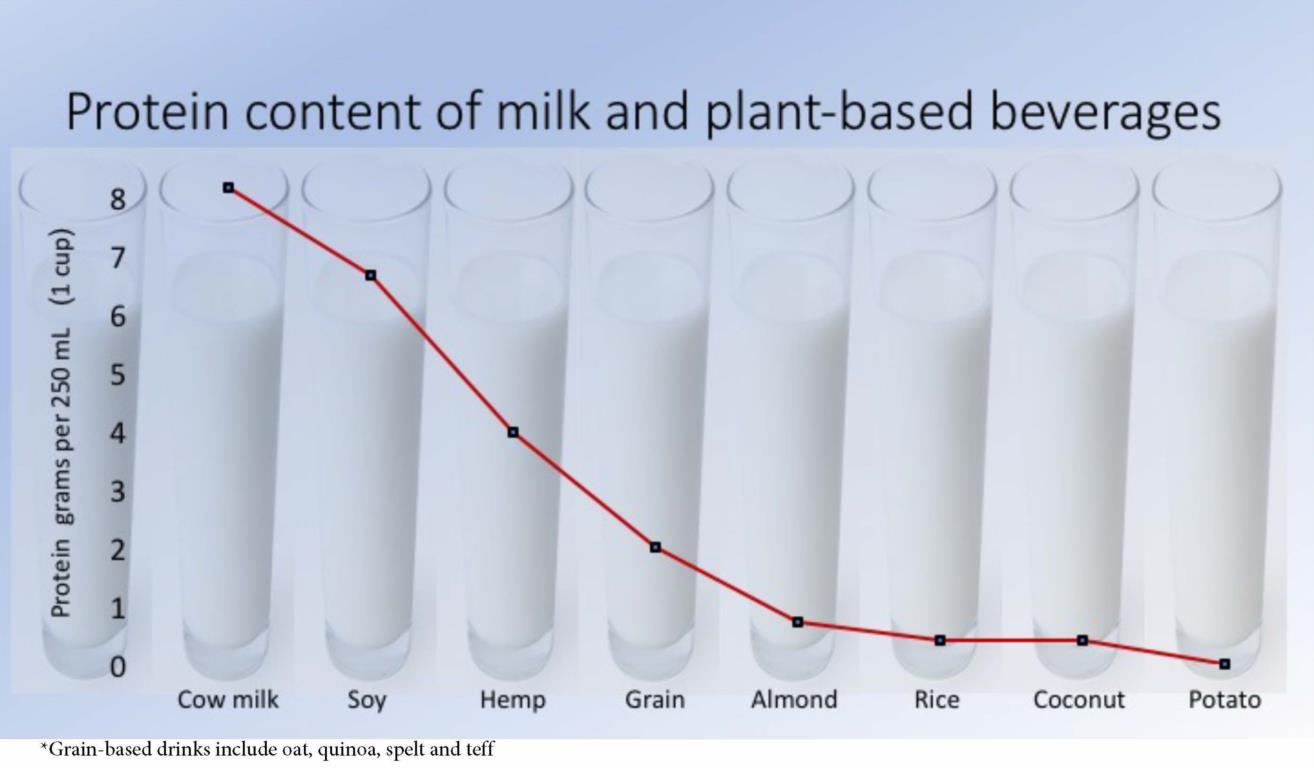
I really appreciated the graphic in this document showing how little protein there is in the various plant-based beverages that are so often described in words that include 'milk' (e.g. almond milk, coconut milk, etc).
What I didn't know was that Health Canada had just issued a requirement earlier this year for manufacturers of plant-based drinks to add the statement "
Not a source of protein" directly on drink containers due to their low protein content, as a way to alert consumers (2). (I don't know if it's a sufficient warning to catch a consumer's attention, but at least it's there for all to read!). The Health Canada document made for more good reading after I finished this article!
References
- Dietitians of Canada. Trending Topics: Plant-based beverages - are they really healthier for young children? In: Practice-Based Evidence in Nutrition [PEN]. 2017 August 29 [cited 2017 Nov 1]. Available from: http://www.pennutrition.com/resourcestools.aspx?trcatid=496&trid=26285&sr=plant-based%2cprotein%2cproteins#. Access only by subscription.
- Health Canada. Interim Policy on the Use of Expired Interim Marketing Authorizations Related to Food Fortification. [cited 2017 Nov 1]. Available from: https://www.canada.ca/en/health-canada/services/food-nutrition/legislation-guidelines/policies/interimpolicy-on-use-expired-interim-marketing-authorizations-related-food-fortification.html#a61
Written by:
Pat Vanderkooy, MSc, RD
Manager Public Affairs
Dietitians of Canada
PEN® Surprising Finding: Migraines and Protein Recommendations for Vegetarian Athletes
Some surprise findings from the nutrition evidence this year for me were:
 That it may be worthwhile for those who suffer from migraines to experiment with identifying and avoiding potential dietary triggers. Although some of the evidence is conflicting, commonly reported dietary triggers included dehydration (up to 91.4%), fasting (up to 82%), drinking alcohol (up to 76%), and cold foods (up to 55.4% of adolescents) (1). This was a surprise given I previously understood that there was no association between food intake and migraines. Despite some of the evidence being conflicting, the association is plausible and therefore a worthwhile test for those who suffer from migraines.
That it may be worthwhile for those who suffer from migraines to experiment with identifying and avoiding potential dietary triggers. Although some of the evidence is conflicting, commonly reported dietary triggers included dehydration (up to 91.4%), fasting (up to 82%), drinking alcohol (up to 76%), and cold foods (up to 55.4% of adolescents) (1). This was a surprise given I previously understood that there was no association between food intake and migraines. Despite some of the evidence being conflicting, the association is plausible and therefore a worthwhile test for those who suffer from migraines.- That as per PEN’s Sports Nutrition - Vegetarianism Knowledge Pathway (2): “Dietary Reference Intakes do not recommend a separate protein intake for vegetarian athletes who consume a variety of complementary plant proteins. The Academy of Nutrition and Dietetics, Dietitians of Canada and the American College of Sports Medicine recommend daily protein intakes of approx. 1.2 to 2.0 g/kg/day for athletes along with sufficient total energy intake to support protein turn over, metabolic adaptions, repair and remodelling. There is no separate protein recommendation for vegetarian athletes”. This was of particular interest as I was recently contacted by one of New Zealand's top tennis players to discuss the potential impacts of switching to a vegetarian diet while playing elite sport. It was helpful to know that although this isn't “A” level evidence, current recommendations suggest that vegetarian athletes should eat the same amount of protein as non-vegetarian athletes. In addition, it was not so surprising that the RDA for iron for vegetarians is 1.8 times that of non-vegetarians and that the EAR may be as much as 30-70% higher for athletes engaged in regular sport (3).
References
- Dietitians of Canada. What dietary components, if any, are triggers for migraine among adults and children who suffer from migraines? In: Practice-Based Evidence in Nutrition [PEN]. 2017 August 9 [cited 2017 Nov 1]. Available from: http://www.pennutrition.com/KnowledgePathway.aspx?kpid=11148&pqcatid=146&pqid=9068. Access only by subscription.
- Dietitians of Canada. Are the protein needs of vegetarian athletes higher than non-vegetarian athletes? In: Practice-Based Evidence in Nutrition [PEN]. 2017 Sep 12 [cited 2017 Nov 1]. Available from: http://www.pennutrition.com/KnowledgePathway.aspx?kpid=14292&pqcatid=146&pqid=4383. Access only by subscription.
- Dietitians of Canada. Are vegetarian athletes at greater risk of iron deficiency than non-vegetarian athletes? In: Practice-Based Evidence in Nutrition [PEN]. 2017 Sep 12 [cited 2017 Nov 1]. Available from: http://www.pennutrition.com/KnowledgePathway.aspx?kpid=14292&pqcatid=146&pqid=4346. Access only by subscription.
Written by:
Rebecca McCarroll
PEN Advisory Council
Dietitians NZ
PEN® Surprising Finding: It Just Makes You Smile
This year I ventured into the field of nutritional psychiatry while supporting an author to develop PEN questions examining nutritional supplements for the prevention or treatment of a mental health disorders. Nutritional psychiatry is a relatively new field of research that recognizes emerging evidence for diet and nutrition as a crucial factor in the prevalence and treatment of mental disorders (1). One of the most exciting studies to come out in 2017 was the SMILES (Supporting the Modification of lifestyle In Lowered Emotional States) Trial, which was really the first intervention study to examine the question ‘if I improve my diet, will my mood improve?’ (2). This Australian study recruited participants from the community who reported experiencing moderate to major depressive symptoms. In the 12-week single-blind RCT, dietitians counselled participants to follow a modified Mediterranean diet (ModiMediDiet) that incorporated principles of the traditional Mediterranean diet from Greece with additional foods commonly consumed in Australia (including red meat and milk) (3). In comparison to a social support control condition, the diet group showed greater improvements in depression scores and greater remission rates (32% versus 8%). The results occurred independent of changes in BMI, smoking or physical activity, but were strongly correlated to the extent of dietary change (2,3).
a mental health disorders. Nutritional psychiatry is a relatively new field of research that recognizes emerging evidence for diet and nutrition as a crucial factor in the prevalence and treatment of mental disorders (1). One of the most exciting studies to come out in 2017 was the SMILES (Supporting the Modification of lifestyle In Lowered Emotional States) Trial, which was really the first intervention study to examine the question ‘if I improve my diet, will my mood improve?’ (2). This Australian study recruited participants from the community who reported experiencing moderate to major depressive symptoms. In the 12-week single-blind RCT, dietitians counselled participants to follow a modified Mediterranean diet (ModiMediDiet) that incorporated principles of the traditional Mediterranean diet from Greece with additional foods commonly consumed in Australia (including red meat and milk) (3). In comparison to a social support control condition, the diet group showed greater improvements in depression scores and greater remission rates (32% versus 8%). The results occurred independent of changes in BMI, smoking or physical activity, but were strongly correlated to the extent of dietary change (2,3).
This study provides evidence for improving diet to treat major depressive episodes, as well as evidence supporting causality. However, the small sample size and inability to blind participants to groups are clear limitations that require additional studies to confirm the results. Importantly, it demonstrates that it is feasible to work with people with mental illness to improve their diets, despite the fatigue and poor motivation that often occurs with depression. Depression also increases the risk of, and is increased by, chronic diseases such as obesity, type 2 diabetes and cardiovascular disease. Improving diet quality of people with depression would also benefit these conditions. The study supports the benefit of adding dietitians to mental health care teams and advocating for the recognition of diet and nutrition as central determinants of mental health.
References
- Sarris J, Logan AC, Akbaraly TN, Amminger GP, Balanzá-Martínez V, Freeman MP, et al; International Society for Nutritional Psychiatry Research. Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry. 2015 Mar;2(3):271-4. doi: 10.1016/S2215-0366(14)00051-0. Epub 2015 Feb 25. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/26359904
- Jacka FN, O'Neil A, Opie R, Itsiopoulos C, Cotton S, Mohebbi M, et al. A randomized controlled trial of dietary improvement for adults with major depression (the 'SMILES' trial). BMC Med. 2017 Jan 30;15(1):23. doi: 10.1186/s12916-017-0791-y. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/28137247
- Opie RS, O'Neil A, Jacka FN, Pizzinga J, Itsiopoulos C. A modified Mediterranean dietary intervention for adults with major depression: Dietary protocol and feasibility data from the SMILES trial. Nutr Neurosci. 2017 Apr 19:1-15. doi: 10.1080/1028415X.2017.1312841. [Epub ahead of print]. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/28424045
Written by:
Dawna Royall, MSc, RD, FDC
PEN
® Senior Evidence Analyst
Dietitians of Canada
PEN® Surprising Finding: The Appendix – A Good Bacteria Storehouse
I’ve long accepted that science relies on an unending process of revision as new information becomes available and supersedes older ideas. For example, when I was in school:
- there were five biological kingdoms (now maybe eight?)
- Pluto was a planet (not anymore… unless you’re in New Mexico or Illinois)
- we did lots of fun experiments that demonstrated the taste map of our tongues (sadly, complete nonsense).
This year I’ve added another revision to my bank of scientific ‘truths’: the appendix is NOT a vestigial organ.
Sure, humans can survive without an appendix, but that doesn’t make it superfluous. Rather than an evolutionary  remnant designed to help our herbivorous ancestors digest plant material, research now suggests the appendix has an important role in humans and other mammals as a reservoir for good bacteria (1).
remnant designed to help our herbivorous ancestors digest plant material, research now suggests the appendix has an important role in humans and other mammals as a reservoir for good bacteria (1).
Diarrhea is never fun, but rapid flushing of the colon can be a helpful defence mechanism in the event that bad bacteria attempt a hostile takeover. Flushing, however, empties the bowel of both harmful and friendly bacteria leaving it open for colonization. That’s where the appendix swoops in. Cleverly positioned outside the stream of fecal matter and therefore protected from flushing, the appendix is a storehouse of good bacteria that helps re-establish normal gut flora (2).
Huh. Who knew? Way to go, appendix.
As demanding as it is to keep an open but critical mind, it’s part of what makes nutrition interesting. Keep your eyes and ears open for the latest scientific revision!
References
- Smith HF, Fisher RE, Everett ML, Thomas AD, Bollinger RR, Parker W. Comparative anatomy and phylogenetic distribution of the mammalian cecal appendix. J Evol Biol. 2009 Oct;22(10):1984-99. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/19678866
- Randal Bollinger R, Barbas AS, Bush EL, Lin SS, Parker W. Biofilms in the large bowel suggest an apparent function of the human vermiform appendix. J Theor Biol. 2007 Dec;249(4):826-31. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/17936308
Written by
Mary Anne Smith, PhD, RD
PEN
® Evidence Analyst
Dietitians of Canada
PEN® Surprising Finding: Gut Microbiome
Last year I was shocked by the concept of fecal transplants. Now over the unpleasant connotations that I initially imagined when hearing this term, I have continued to be surprised (in a positive way) by the emerging evidence for the role of the gut
microbiome in health. With increasing rates of obesity and chronic disease globally, it's exciting to hear about the role the gut microbiome may play in a range of conditions including mental health, diabetes and obesity. While many studies to date have been observational or in animals, the results provide support for future research in this space. The findings may add another piece to the puzzle in understanding and managing these complex, chronic conditions.
The studies researching the link between weight and the gut microbiome, I have found most fascinating. A 2016 review investigated the role of the gut microbiota in obesity (1). This review included studies that compared the differences in microbiome in those who are lean and those who are obese. It also looked at a number of studies identifying the role of the gut microbiome in metabolism, hormones and inflammation; all possible mechanisms to explain how the gut microbiota may play a role in obesity. There has also been a fascinating study from Israel investigating the impact that yo-yo dieting has on the gut bacteria of mice, providing possible explanation as to why maintaining weight loss is so difficult (2). While there is no conclusive evidence at this stage, it is interesting to learn of another potentially modifiable factor in weight management. Could interventions to improve gut health become part of regular dietetic practice for weight management in the future? It is exciting to imagine the possibilities that may come from more research.
What I find most promising about this emerging evidence is the potential role that diet can play in modifying the gut bacteria. These changes in microbiome can take place in a short time frame (3). Dietitians globally will play a vital role in this space moving forward. We may even be individualizing diets down the track based on one's gut microbiome. I look forward to hearing more advancements in this area and seeing what it means for the future practice of dietitians.
References
- Khan MJ, Gerasimidis K, Edwards CA, Shaikh MG. Role of gut microbiota in the aetiology of obesity: proposed mechanisms and review of the literature. J Obes 2016;2016:7353642. Epub 2016 Sep 15. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/27703805
- Thaiss CA, Itav S, Rothschild D, Meijer M, Levy M, Moresi C, et al. Persistent microbiome alterations modulate the rate of post-dieting weight regain. Nature. 2016 Nov 24. doi: 10.1038/nature20796. [Epub ahead of print]. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/27906159
- David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet rapidly and reproducibly alters the human gut microbiome Nature. 2014 Jan 23;505(7484):559-63. doi: 10.1038/nature12820. Epub 2013 Dec 11. Abstract available: https://www.ncbi.nlm.nih.gov/pubmed/24336217
Written by:
Natalie Stapleton, APD
Manager Professional Services
Dietitians Association of Australia
PEN® Surprising Finding: Mouth Rinsing and Sports Performance
I have always found sports nutrition fascinating. The synergy between muscle action, nutrients and hormones on a foundation of physiology and biochemistry has always held great interest for me. I love my job as the PEN Editor, but

I think I could also be happy being the New England Patriots Dietitian and having chats with Tom Brady about his dietary views and habits.
The Sports Nutrition Knowledge Pathway was recently updated. Although I enjoyed editing the hundreds of pages of content, one piece of evidence that really caught my attention was the use of mouth rinsing and its impact on sports performance:
“Receptors in the mouth coming in contact with carbohydrate (CHO), via either mouthwash or oral consumption (providing there is adequate oral contact time), can stimulate the pleasure and reward centers of the brain, and via a central nervous system (CNS)-based mechanism, can improve exercise performance, including that which is one hour or less in duration” (1).
The idea that stimulating the pleasure and reward centers of the brain via nutrient consumption can result in an improvement in exercise performance is really fascinating. Additional details include (1):
- The amount that was deemed effective was approximately 1.5 g CHO in 25 mL for five to 10 seconds every eight to 10 minutes of exercise.
- Performance benefits were seen even when the athletes had recently eaten.
- Functional MRI brain imaging research found that both sweet (such as glucose) and non-sweet CHO (such as maltodextrin) mouth rinsing activated pleasure and reward areas of the brain and those associated with motor control as well.
- In addition to improvement in performance, the CHO mouth rinsing improved ratings of perceived exertion (RPE) in both time trials and time to exhaustion protocols.
- The performance benefits were seen in events lasting one hour or less. This and the above evidence from MRI and RPE supports a neural mechanism for the mouth rinsing, versus metabolic mechanism.
- The Academy of Nutrition and Dietetics, Dietitians of Canada and the American College of Sports Medicine concluded in their 2016 position paper that mouth rinsing can be recommended. They stated that carbohydrate intake is not necessary during brief exercise (such as 45 minutes or less) but that during sustained high intensity exercise lasting 45-75 minutes, small amounts of CHO, including mouth rinses, can be recommended.
- It has been acknowledged that during competition it may not always be practical to use CHO mouth rinsing protocols and that the five to 10 seconds of rinsing could impact the athlete’s ability to breathe heavily enough to support effort. Experts suggested a sports confectionary in the cheek cavity as a possible solution.
Athletes in competitive sports are always looking for that “edge” and as dietitians we have much to offer. We understand the function of the individual nutrients, but more importantly, we understand how nutrients interact together and how they interact as part of body systems and body functioning. As dietitians, we have the education, training and skills to take evidence-based information and position it in the best interests of our clients, whether individual or population.
References
- Dietitians of Canada. What are the effects of consuming carbohydrate during exercise that lasts approximately one hour or less? In: Practice-Based Evidence in Nutrition [PEN]. 2017 October 23 [cited 2017 Nov 8]. Available from: http://www.pennutrition.com/KnowledgePathway.aspx?kpid=8180&pqcatid=146&pqid=11977. Access only by subscription.
Written by:
Heather Alaverdy, MA, RD
PEN
® Editor
Dietitians of Canada
PEN® Surprising Finding: Sweating Blood and Artificial Intelligence
I’ve had a busy year. I found myself describing one of my bigger projects to a friend I hadn’t spoken to in a while. “I’ve really

sweat blood over this one”, I told her, hoping my metaphor helped emphasize the hours of effort it had taken me to sort through the complexities of the project. I recalled this conversation when I scanned a
recent newsfeed about hematohidrosis. The saying “sweating blood” was one I’d picked up from my mother and I’m certain she had never heard of hematohidrosis. She was just a hardworking woman fond of quaint sayings. What is really fascinating is that this recent case has both doctors and medical historians puzzling over it. Documented by Aristotle and often associated with religious writings, Duffin noted 28 new case reports in the medical literature since 2004 (1). Predominantly occurring in young females, clinicians don’t agree on the etiology, and while frightening to experience, no one appears to have died of the condition. To read more about this unusual condition see:
Duffin J. Sweating blood: history and review. CMAJ. 2017 Oct 23;189.42:1315.
Maglie R, Caproni M. A case of blood sweating: hematohidrosis syndrome. CMAJ. 2017 Oct 23;189(42):E1314. doi: 10.1503/cmaj.161298.
Now that I have your attention, here is what I really wanted to share as my interesting or surprising finding:
PEN® Surprising Finding: How will Artificial Intelligence (AI) Assist Dietitians and Nutritionists?
AI will speed up our ability to systematically examine the research literature and put important findings into practice quicker. Check out the short video on the Cochrane.org site to learn more. What is really thrilling is that they are already working on nutrition topics!
References
- Duffin J. Sweating blood: history and review. CMAJ. 2017 Oct 23;189.42:1315. Link not available.
Written by:
Jayne Thirsk RD, PhD, FDC
Director, PEN
®
Dietitians of Canada
PEN® Surprising Finding: Non-celiac Gluten Sensitivity (NCGS) and Gluten Restriction Do people with non-celiac gluten sensitivity (NCGS) need to restrict gluten?
The answer is maybe not. Based on new research from Oslo Norway, fructans, not gluten, may be the culprit; but foods with gluten often contain fructans, a type of fermentable oligo-, di-, monosaccharides and polyols (1). Fructans are  found in wheat and rye but also in other foods like avocados, artichokes, asparagus, leeks, garlic, and onions. Non-celiac gluten sensitivity has been a puzzle for some time as there are no biomarkers for the disorder. In people with gluten sensitivity, who have had it confirmed that they do not have celiac disease, symptoms improve after the removal of gluten from the diet.
found in wheat and rye but also in other foods like avocados, artichokes, asparagus, leeks, garlic, and onions. Non-celiac gluten sensitivity has been a puzzle for some time as there are no biomarkers for the disorder. In people with gluten sensitivity, who have had it confirmed that they do not have celiac disease, symptoms improve after the removal of gluten from the diet.
It is estimated that one percent of the world-wide population has celiac disease. Another 16% claim to have a sensitivity or intolerance to gluten responding when gluten was removed from the diet and only 0.10 percent of those living in Westernized countries are believed to have a wheat allergy. “International consensus statements have defined non-celiac gluten sensitivity (NCGS) as a condition in which ingestion of gluten induces gastrointestinal and extra-intestinal symptoms in absence of celiac disease or wheat allergy (2).”
This recent double-blind crossover challenge aimed to confirm the effect of gluten versus fructans separately in 59 adults who self-reported being sensitive to gluten (1). The participants were randomly assigned to groups and placed on seven- day diets “containing gluten (5.7 g), fructans (2.1 g), or placebo, concealed in muesli bars. Following a minimum seven-day washout period (until the symptoms induced by the previous challenge were resolved), participants crossed over into a different group, until they completed all three challenges (gluten, fructan, and placebo). Symptoms were measured by gastrointestinal symptom rating scale irritable bowel syndrome (GSRS-IBS) version”.
The GSRS-IBS scores varied significantly during the three challenges: gluten, fructans and placebo. The GSRS-IBS score for participants consuming fructans was “significantly higher than for participants consuming gluten (P=0.049), as was the GSRS bloating score (P=0.003). Thirteen participants had the highest overall GSRS-IBS score after consuming gluten, 24 had the highest score after consuming fructan, and 22 had the highest score after consuming placebo. There was no difference in GSRS-IBS scores between gluten and placebo groups”.
Implications for Practice: While this research generally found no effect of gluten on those with self-reported NCGS, who were sensitive to wheat, rye and barley; fructans were more likely to induce gastrointestinal symptoms. The findings question the use of the term “NCGS” and raises doubts about the need for a gluten-free diet in this population. The research on fructans is still in the early stages and the numbers of subjects has been small, so no practice changes can be recommended at the moment, but certainly something to keep an eye on.
References
- Skodje GI, Sarna VK, Minelle IH, Rolfsen KL, Muir JG, Gibson PR, et al. Fructan, rather than gluten, induces symptoms in patients with self-reported non-celiac gluten sensitivity. Gastroenterol. 2017. doi: 10.1053/j.gastro.2017.10.040. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/29102613
- Leonard MM, Sapone A, Catassi C, Fasano A. Celiac disease and nonceliac gluten sensitivity: a review. JAMA. 2017 Aug 15;318(7):647-56. doi: 10.1001/jama.2017.9730. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/28810029
Written by:
Beth Armour, MEd, P.Dt
PEN
® Content Manager
Dietitians of Canada