PEN® eNews 15(5) May 2025 - New Guidelines for the Management of Pediatric Obesity
PEN
® eNews is a monthly e-newsletter shared with the global PEN Community and created to help dietitians position themselves as leaders in evidence-based nutrition practice. In addition, users of the PEN System will find articles on the new evidence, resources and features available and how to maximize one's use of PEN.
How Should Dietitians Advise Families and Caregivers of Children Living With Obesity?
The content in this PEN Practice Question has incorporated the recommendations of new national Clinical Practice Guidelines for Managing Obesity in Children.
The Question
Does family and/or caregiver involvement result in improved outcomes for children and adolescents with overweight and obesity? How should dietitians advise families or caregivers of children and adolescents with overweight and obesity?
Recommendation
The optimal role of the parent(s) and caregiver(s) in their child or adolescent’s obesity management is not clear. Evidence suggests that interventions targeting children and adolescents (aged six to 18 years) are equally effective when they involve parents as when they do not.
Contact time between the health care provider and the parent does not influence the effectiveness of behavioural interventions to treat overweight and obesity in children. Dietitians can implement the following good practices when interacting with families: use person-first language; establish a positive, non-judgmental relationship; use neutral terms (e.g. weight, BMI, growth) to discuss growth chart findings; consider social determinants to health and barriers to care; consider using a framework to identify broad outcomes of obesity management interventions; encourage family involvement using a non-stigmatizing approach; consider using a framework to facilitate family conversations; work in multidisciplinary teams where possible; and consider all type of interventions (behavioural, psychological, pharmacological, surgical) using shared decision-making. Offering interventions that consider family/ caregiver needs as well as the child's needs (e.g. facilities and times that are convenient for working family members and other children in the household) can increase adherence to the intervention.
Parent or caregiver attendance at counselling sessions may be less important with adolescents than with children. If the adolescent is a capable decision-maker, he or she should be treated as such. However, health behaviours of the whole family, rather than weight, should be the focus of intervention in adolescents.
Remarks
Parents and caregivers may not recognize overweight or obesity in their children. This topic may need to be introduced to and discussed with the family using a non-judgmental approach before treatment strategies can be implemented. Strategies are discussed in the Comment section.
Most (90%) studies of interventions targeting parents and/or caregivers in the management of their child’s overweight or obesity do not report on implementation rates of the intervention. If parents do not implement the intervention as designed, this can confound assessment data.
To see the full practice question, including the Evidence Statements, Remarks and References, click here.
What Outcomes Should Be Used to Determine the Effectiveness of Treatment for Children Living With Obesity?
The content in this PEN Practice Question has incorporated the recommendations of new national Clinical Practice Guidelines for Managing Obesity in Children.
The Question
What outcomes should dietitians use to determine the effectiveness of treatment for children and adolescents with obesity?
Recommendation
Recent Canadian guidelines prioritize the following outcomes of pediatric obesity management interventions, taking patient and caregiver values into account:
Critically important: health-related quality of life, depression, anxiety, serious adverse events
Very important: weight, BMI, BMI z-score (i.e. change in BMI over time), mild/ moderate adverse events
Important: biochemical measures (e.g. blood pressure, cholesterol, insulin resistance)
British guidelines add dietary and physical behaviours as important outcomes to measure, along with process outcomes (e.g. e.g. number of children participating, dropout rate, percentage of participants lost to follow-up) for group interventions.
From a research perspective, obesity status should be a primary research outcome when determining the effectiveness of obesity treatment programs in children and adolescents. It is suggested that obesity should be measured using BMI and, if available, dual-energy X-ray absorptiometry (DeXA). Relevant secondary research outcomes should be tailored to the aims of the intervention and may include: diet, eating behaviours, physical activity, sedentary behaviour, fitness (i.e. aerobic capacity, muscular strength, muscular endurance), psychological well-being, health-related QOL, environment and physiological measures.
Remarks
DeXA is not routinely available for clinical purposes and its use may be more feasible when used in a research context to verify the accuracy of BMI classification. DeXA measurements corresponding with overweight and obesity vary according to age, sex, fat mass and nutritional status. No gold standard tool was identified to measure eating behaviours. When dietary intake is measured, food frequency questionnaires (FFQs) are suggested as being more valid than food diaries or food recalls in children with obesity. FFQs should be tested for validity and reliability; the most recommended FFQs for this population include: the Short Youth Adolescent Questionnaire, the Youth Adolescent Questionnaire, the Children’s Eating Habits Questionnaire, the Australian Child and Adolescent Eating Survey, the Diet Fat Screening Measure and the New Zealand FFQ.
To see the full practice question, including the Evidence Statements, Remarks and References, click here.
Do Weight Management Interventions Increase Eating Disorder Risk in Children and Adolescents?
The content in this PEN Practice Question is important for practitioners considering implementing interventions to manage obesity in children and adolescents.
The Question
Do interventions to prevent or treat obesity put children and adolescents at risk for disordered eating and/or other harms?
Recommendation
Adverse events such as eating disorders, compromised linear growth and psychological harms are poorly reported in studies examining weight management interventions in children and adolescents (aged two to 18 years). Currently, evidence does not suggest that weight management interventions increase the risk of harm in children or adolescents with overweight or obesity.
On the contrary, there is limited evidence to suggest that combined diet, exercise and behavioural/psychological interventions may improve depressive symptoms, body satisfaction and decreased internalization of female norms, and decrease disordered eating behaviours.
To mitigate any potential risk that may not yet have been identified, national and international guidelines recommend that weight management interventions in children and adolescents include ongoing evaluation of psychological well-being and be delivered by multidisciplinary professional teams with appropriate training regarding weight-related stigmatization.
Remarks
Children and adolescents with overweight or obesity may be more likely to use extreme weight-control behaviours, and restrictive eating disorders (e.g. anorexia nervosa) may be less recognized in this population than in their normal-weight peers. Children and adolescents with overweight or obesity are also more likely to be teased or bullied than their normal-weight peers, both of which are significant risk factors for the development of eating disorders or unhealthy weight-control behaviours. It is not known whether disordered eating is a cause or consequence of childhood obesity.
To see the full practice question, including the Evidence Statements, Remarks and References, click here.
Did You Know?
Ever wonder what a "Practice Question" is, or why PEN is organized in the way that it is? Our Terminology and Features page will help make this clearer for you.
The first section of the page gives brief descriptions of common terminology found in PEN. For example, a “Practice Question” reflects the everyday practice situations faced by dietitians and is generally formulated using the PICO approach (Population, Intervention, Comparison, Outcome). Our “Recommendations” are clear, concise and actionable advice on whether to implement an intervention and, if relevant, under what conditions and how.
The next section of the page lists the key features of PEN and tells the reader what you can expect each feature to do for you. For example, if you have a suggestion for new content that should be included in PEN, using the “Submit a Content Idea” feature enables you to contribute to the PEN System’s database to build future content for the service.
If you’re new to PEN, or just want to explore parts of the website that you weren’t aware of before, our Terminology and Features page is a great place to start!
To see the Terminology and Features page, click here.
Find Last Month's PEN eNews
Have you ever wanted to revisit an issue of PEN eNews, but deleted the email from your inbox and don't know how to find it again? Here is a quick tour through the website to show you where to find both current and archived issues of PEN eNews.
First, open the navigation menu at the top of the screen. Then, click “PEN eNews Issues”.
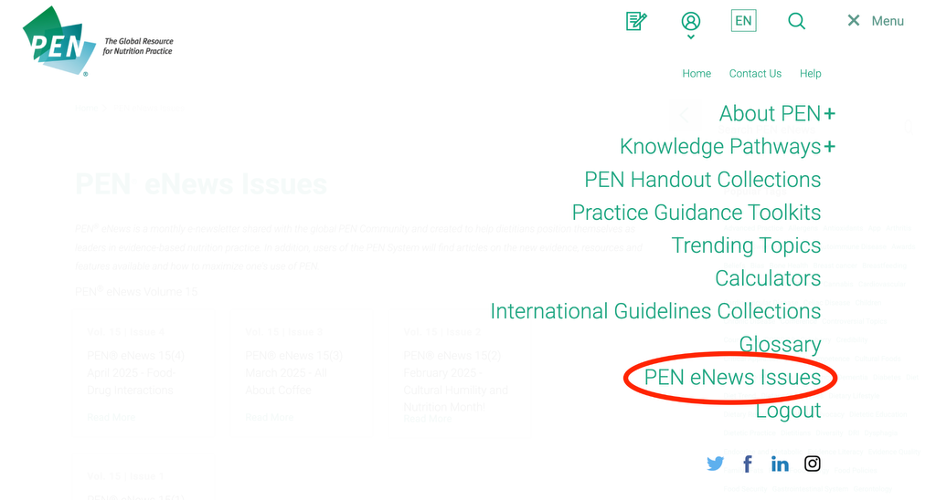
That’s it! If you forget, you can always click this direct link.
Happy reading from the PEN team!
PEN eNews
May 2025 Volume
15 (5)
A Publication of the PEN® System Global Partners,
a collaborative partnership between International Dietetic Associations.
Learn more about PEN.
Copyright Dietitians of Canada
. All Rights Reserved.