eNews is a monthly e-newsletter shared with the global PEN Community and created to help dietitians position themselves as leaders in evidence-based nutrition practice. In addition, users of the PEN System will find articles on the new evidence, resources and features available and how to maximize one's use of PEN.
The PEN System showcased at Dubai International Nutrition Congress
On October 24-26, 2018, I was delighted to be invited by the scientific and organizing committee to attend, participate and present at the 4th Dubai International Nutrition Congress (DINC). I presented a session on «Clinical  Nutrition Management Challenges » and on behalf of the PEN (Practice-based Evidence in Nutrition) System, I also offered a workshop and shared through the 3-day conference how the PEN system can support dietitians (clinicians, practitioners, academics and students) and other healthcare professionals to be evidence-based practitioners in the Middle East Region.
Nutrition Management Challenges » and on behalf of the PEN (Practice-based Evidence in Nutrition) System, I also offered a workshop and shared through the 3-day conference how the PEN system can support dietitians (clinicians, practitioners, academics and students) and other healthcare professionals to be evidence-based practitioners in the Middle East Region.
Dubai International Nutrition Congress (DINC) was hosted by the Dubai Health Authority in United Arab Emirates (UAE) and attracted key leaders and experts in the field of nutrition and dietetics from UAE, other GCC (Gulf Cooperation Council) countries such as Saudi Arabia, Kuwait, Bahrain, Oman, Qatar but also attendees from Jordan, Egypt and many from my birthland Lebanon. DINC featured a wide range of scientific sessions by national and international speakers on clinical and community nutrition and food science.
A few of the topics highlighted over the course of the three days are topics also covered in PEN:
-
Ketogenic Diet and Cancer
-
Nutrition and wound care management
-
Reality of prebiotics and healthy gut
-
Popular weight loss diet: review and evidence
-
Herbal remedies and women health during menopause
-
Food Allergies
-
Nutrition counseling in the treatment of eating disorders
-
Bariatric surgery
-
Weight perception: the hidden aspect in childhood obesity
-
Sports nutrition
The global nutrition community is managing many of the same nutritional issues such as malnutrition, diabetes, obesity, allergic disease, eating disorders, cancer and gut disease. As dietitians and health care professionals, we face the continuing challenge of how to quickly access the rapidly expanding nutrition evidence base and locate the best tools and resources necessary to help us apply that evidence into our practices.
One of my roles at DINC was to introduce and help participants of the Middle East region to become familiar with the key features of the PEN system, understand how the PEN system evaluates the quality of evidence, experience how PEN supports evidence-based practice in a variety of settings and encourage them to participate in the PEN Community because they have no other similar resources available in the region. Feedback received was that the PEN System provides simple access to timely, current and authoritative guidance on food and nutrition topics. It offers evidence-based answers to the questions encountered in every day practice.
This congress was an excellent opportunity for all participants from different middle eastern countries and specialties to discover the value of PEN Nutrition.
By working together, the PEN global system has created a relevant and sustainable evidence base that demonstrates the value of nutrition and dietetics around the world. Adopted by a growing number of nutrition and dietetic associations, I encouraged dietitians and key leaders in nutrition from the UAE, middle east and gulf region to join the
PEN system and to enhance their evidence-based practice.
The PEN team monitored usage statistics from 10 selected countries known to have representatives in attendance at the congress. We noted a spike in the number of free trials and welcome our colleagues from the Middle East Region.
Written by:
Mireille Najm, RD, MS
PEN® Surprising Findings 2018
Dating Profile: Must Love Gluten-free Diets? (Or at least the dieter)
Mediterranean Diet Retraction
Are you ready to print your food?
When is a diet not a diet?
Omega-3’s and Cardiovascular disease
Surprising findings about vitamin D and fish oil – maybe you don’t need supplements?
PEN System is definitely “making the GRADE”
Time Flies
Calcium Supplementation and PMS
Using levies to improve eating behaviours
Primary and Secondary CVD Prevention and Daily Fish Intake – Wow!
Surprising findings about Fluoride
Nutritional considerations for transgender people
Dating Profile: Must Love Gluten-free Diets? (Or at least the dieter)
As most dietitians are aware, gluten-free diets are not just for those with Celiac disease. It has been estimated that,  worldwide, millions of people intentionally follow a gluten-free diet even without Celiac disease (1). The dietary practice is so popular that it is no longer just an area of research for medical or nutritional sciences. A very interesting study (titled “Too Picky for My Tastes?...”) recently published in the social sciences explored the concept of a consumption stereotype with regards to those who follow a gluten-free diet and how might that impact impression formation and dating interest.
worldwide, millions of people intentionally follow a gluten-free diet even without Celiac disease (1). The dietary practice is so popular that it is no longer just an area of research for medical or nutritional sciences. A very interesting study (titled “Too Picky for My Tastes?...”) recently published in the social sciences explored the concept of a consumption stereotype with regards to those who follow a gluten-free diet and how might that impact impression formation and dating interest.
In the dating context, those following a gluten-free diet were viewed by non-dieters as more likely to be picky, demanding, selfish, entitled, arrogant, difficult to please, high-maintenance, judgmental and complaining but also as more self-disciplined, moral, healthy, confident, intelligent, understanding and energetic. Following a gluten-free diet was viewed as more associated with femininity and judgments of men following a gluten-free diet were more negative than those of women who were following it. There was initially some hesitation by survey participants to date those following a gluten-free diet, but in the end, no difference was observed in a mock dating experiment when presented with potential romantic partners’ dating profile.
I find studies that merge nutritional science and social science topics together as these investigators have done to be very intriguing. Such research can have important implications for dietitians; from impacting nutrition counseling to message development and more. I look forward to reading additional novel, cross-field research studies such as this one in the future.
Written by:
Heather Petrie, MSc, RD
PEN® Evidence Analyst
Reference
- Aloni M, Geers AL, Coleman M, Milano K. Too picky for my taste? The effect of the gluten-free dietary restriction on impressions of romantic partners. Appetite. 2018 Sep 15. pii: S0195-6663(18)30008-4. doi: 10.1016/j.appet.2018.09.012. [Epub ahead of print]. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/3022718
Mediterranean Diet Retraction
A landmark study on the Mediterranean diet (PREDIMED trial) made news this year as 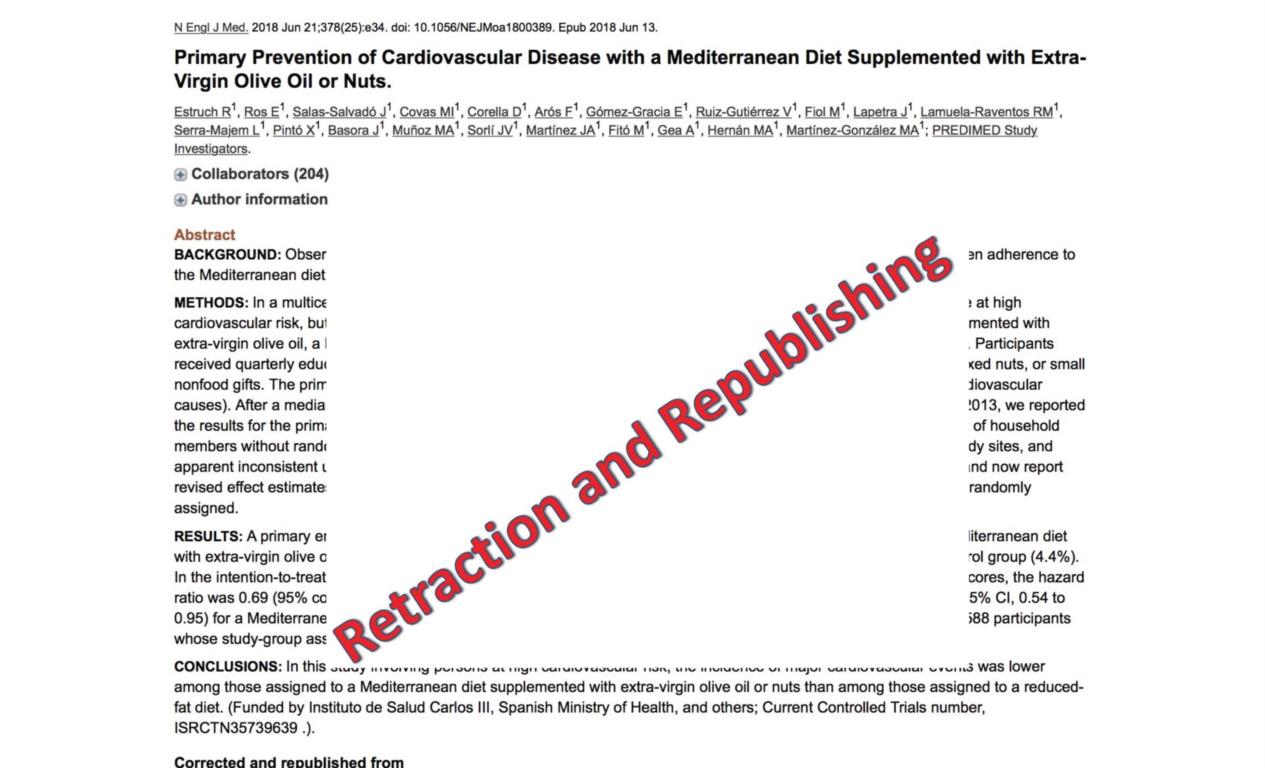 the #1 most highly cited retracted paper on Retraction Watch (1). The PREDIMED trial was a diet study on 7500 people in Spain, which reported that eating a Mediterranean diet supplemented with olive oil and nuts could reduce cardiovascular disease events by 30%. The New England Journal of Medicine retracted and then republished the study (2). PEN reported on this as a Trending Topic (Update on the Mediterranean Diet).
the #1 most highly cited retracted paper on Retraction Watch (1). The PREDIMED trial was a diet study on 7500 people in Spain, which reported that eating a Mediterranean diet supplemented with olive oil and nuts could reduce cardiovascular disease events by 30%. The New England Journal of Medicine retracted and then republished the study (2). PEN reported on this as a Trending Topic (Update on the Mediterranean Diet).
The physician behind the retraction was John Carlisle who applied statistical tests to scrutinize over 5000 RCTs across eight journals published from 2000-2015. Basically, for experiments in which people are randomly assigned to different groups, the characteristics of the groups should be similar before the trial begins. Carlisle used statistical tests to identify whether the distribution of height, weight, age and other factors were implausible, resulting in a non-random assignment of volunteers to different treatments. The PREDIMED trial was flagged as suspicious. Digging up records from the start of the trial, the researchers uncovered that up to 1588 people hadn’t been properly randomized: some people were assigned to the same diet as someone else in their household, some people in rural areas were assigned to different diets based on proximity to a clinic. The authors reanalyzed the data and found that the conclusions were the same, but with less statistical power than the original paper. Of concern is the fact that the original 2013 landmark study has been cited over 1900 times in other articles (1). There have also been several other post hoc analyses published from the original PREDIMED trial, many of which are now having errata published (http://www.predimed.es/publications.html).
Although retractions are pretty rare (minor corrections are more common), they are concerning. I take heart in the fact that journal editors and authors are more open to the possibility of questioning data, and willing to allow people to look at their data to identify and correct errors. Let’s continue to look at research critically and examine individual studies in the context of the entire body of evidence.
Written by:
Dawna Royall, MSc, RD, FDC,
PEN Senior Evidence Analyst
References
- Retraction Watch. The 10 most highly cited retracted papers; October 2018 [cited 2018 Nov 8]. Available from: http://retractionwatch.com/the-retraction-watch-leaderboard/top-10-most-highly-cited-retracted-papers/
- Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al.; PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018 Jun 21;378(25):e34. doi: 10.1056/NEJMoa1800389. Epub 2018 Jun 13. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/29897866
Are you ready to print your food?
When I was young, I used to spend a lot of time thinking up far-fetched inventions and writing them out in great detail.  One summer afternoon I “invented” a printer which could “print” real food for consumption. The concept was that anything that could be drawn in Microsoft Paint could be printed – the possibilities would be endless! I guess the idea wasn’t so far-fetched after all because 3D printing of food has been actualized, and it appears to have broad potential.
One summer afternoon I “invented” a printer which could “print” real food for consumption. The concept was that anything that could be drawn in Microsoft Paint could be printed – the possibilities would be endless! I guess the idea wasn’t so far-fetched after all because 3D printing of food has been actualized, and it appears to have broad potential.
3D printing is an additive manufacturing process which builds objects by depositing a printing medium in layers to create three dimensional objects designed using a computer-aided design (CAD) software (1). Similarly, for food 3D printing, the printer’s syringe-like container is filled with ingredients (e.g. edible powders, gels, sugars, doughs) which are deposited as layers on top of one another to create food products (1). Food 3D printing can have many applications. Some of the early adopters of this technology are using it to produce foods tailored to specific nutritional needs, such as forming vegetable purees into more appetizing-looking meals for those with chewing difficulties (2). Not only does 3D food printing boost culinary creativity, it offers the potential of nutrient and ingredient customizability and food sustainability (1).
At present, food 3D printing is still in its infancy. It will surely be interesting to see the progression of this technology and its applications in the field of nutrition, food and health care.
PEN has a Background document in the works for 2019 on this topic!
Written by:
Noor Naqvi
PEN Evidence Analyst
References
- Reichental A. How 3-D Printing Is Revolutionizing The Concept Of Food [Internet]. Forbes. Forbes Magazine; 2018 [cited 2018 Nov 16]. Available from: https://www.forbes.com/sites/forbestechcouncil/2018/05/21/how-3-d-printing-is-revolutionizing-the-concept-of-food/#519634ff1e60
- CBS News. Nursing homes in Germany serve 3D-printed food [Internet]. CBS News. CBS Interactive; 2014 [cited 2018 Nov 16]. Available from: https://www.cbsnews.com/news/nursing-homes-in-germany-serve-3d-printed-food/
When is a diet not a diet?
I have always had a particular interest in breast cancer research as my first role as a research dietitian was setting up  a study looking at a very low fat diet for women previously diagnosed with breast cancer. I was interested to read about research done by Dr Michelle Harvey’s group in Manchester, England. I knew from my own work that women who have previously had a breast cancer diagnosis and have been advised to lose weight to improve their health post treatment often find it hard to achieve and maintain weight loss. Previous research in Manchester had shown that intermittent energy restriction comprising two days of low energy intake and the remaining five days on a Mediterranean diet resulted in better insulin profiles and adipose tissue loss in this group than those randomised to the other arm which comprised a calorie restricted Mediterranean diet . What surprised the group was the “carry over effect”, the intermittent energy restricted group reduced their energy intake by 25% on the “other” days. A new study was conducted to investigate this phenomenon using a qualitative methodology. The study participants had all been in the intermittent energy restricted arm of the previous trial, women who has lost 5% of their body weight were compared with those who had been unsuccessful. The researchers found three themes; “(i) redefining dieting; (ii) the impact of intermittent dieting on normal eating behaviour and diet adherence; and (iii) reduced cognitive complexity with the intermittent diet”. The results in theme (i) suggest that the women viewed the 2 days as “dieting days” and the other 5 as non-dieting days even though the healthy Mediterranean diet was healthier and lower in energy than their previous “normal” diet.
a study looking at a very low fat diet for women previously diagnosed with breast cancer. I was interested to read about research done by Dr Michelle Harvey’s group in Manchester, England. I knew from my own work that women who have previously had a breast cancer diagnosis and have been advised to lose weight to improve their health post treatment often find it hard to achieve and maintain weight loss. Previous research in Manchester had shown that intermittent energy restriction comprising two days of low energy intake and the remaining five days on a Mediterranean diet resulted in better insulin profiles and adipose tissue loss in this group than those randomised to the other arm which comprised a calorie restricted Mediterranean diet . What surprised the group was the “carry over effect”, the intermittent energy restricted group reduced their energy intake by 25% on the “other” days. A new study was conducted to investigate this phenomenon using a qualitative methodology. The study participants had all been in the intermittent energy restricted arm of the previous trial, women who has lost 5% of their body weight were compared with those who had been unsuccessful. The researchers found three themes; “(i) redefining dieting; (ii) the impact of intermittent dieting on normal eating behaviour and diet adherence; and (iii) reduced cognitive complexity with the intermittent diet”. The results in theme (i) suggest that the women viewed the 2 days as “dieting days” and the other 5 as non-dieting days even though the healthy Mediterranean diet was healthier and lower in energy than their previous “normal” diet.
Read more about this study in the Journal of Human Nutrition and Dietetics: https://onlinelibrary.wiley.com/doi/full/10.1111/jhn.12571
Watch for PEN content on intermittent fasting in 2019.
Written by:
Judy Lawrence, RD, PhD
PEN® Evidence Analyst
Research Officer
British Dietetic Association
Omega-3’s and Cardiovascular disease
Historically we’ve seen subgroups of the population such as the Inuit’s with higher intakes of fish, experience lower levels  of cardiovascular disease. Observational studies have often suggested a relationship between omega-3 intake and cardiovascular disease. This has potentially contributed to the strong public belief that omega- 3 supplementation offers benefit for cardiovascular disease and the resulting high intake of these supplements. This belief has often been maintained despite key national guidelines and recommendations, such as the NICE guidelines (1), encouraging fish intake but not supplementation with omega-3. This highlights the potentially disjoint we see often between the evidence and recommendations and the public’s belief.
of cardiovascular disease. Observational studies have often suggested a relationship between omega-3 intake and cardiovascular disease. This has potentially contributed to the strong public belief that omega- 3 supplementation offers benefit for cardiovascular disease and the resulting high intake of these supplements. This belief has often been maintained despite key national guidelines and recommendations, such as the NICE guidelines (1), encouraging fish intake but not supplementation with omega-3. This highlights the potentially disjoint we see often between the evidence and recommendations and the public’s belief.
This year we saw the release of an updated Cochrane systematic review- Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease (2). This review included high quality trials investigating the effect of omega-3 on cardiovascular disease in more than 110,000 people from many countries around the globe. The review found little to no benefit of Omega-3 in cardiovascular disease. This high quality review received significant public attention worldwide and will hopefully help lead to a change in the public’s belief on the perceived benefits of omega- 3 supplementation.
For me this review continued to highlight the importance of considering dietary patterns in disease prevention and management. Individuals and populations don’t eat nutrients in isolation and as dietitians it’s crucial we continue to consider the role of dietary patterns and environments in health.
Written by:
Natalie Stapleton, APD
Senior Manager Professional Services and PEN Evidence Analyst
Dietitians Association of Australia
References:
- NICE Guidelines NICE. Cardiovascular disease: risk assessment and reduction, including lipid modification Clinical guideline [CG181]. www.nice.org.uk/guidance/cg181 July 2014, last updated September 2016.
- Cochrane: Abdelhamid AS, Brown TJ, Brainard JS, Biswas P, Thorpe GC, Moore HJ, Deane KHO, AlAbdulghafoor FK, Summerbell CD, Worthington HV, Song F, Hooper L. Omega 3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database of Systematic Reviews 2018, Issue 7. Art. No.: CD003177. DOI: 10.1002/14651858.CD003177.pub3.
Surprising findings about vitamin D and fish oil – maybe you don’t need supplements?
Just when I was thinking I should get serious about taking a vitamin D supplement and some cod liver oil this winter,  I read a few papers that have me second guessing this idea. It appears there is no evidence to show added value for health or to prevent disease by taking these supplements. And that surprised me! Consider these studies:
I read a few papers that have me second guessing this idea. It appears there is no evidence to show added value for health or to prevent disease by taking these supplements. And that surprised me! Consider these studies:
Preliminary results from a 3-year Canadian investigation into varying doses of vitamin D and the effect on bone health were shared by researchers from the University of Calgary at two recent conferences (1,2). In this double-blind randomized clinical trial, 373 participants aged 55 to 70 years (with serum 25hydroxyvitamin D level between 30 nmol/L and 125 nmol/L) were randomly assigned to take 400 IU, 4,000 IU or 10,000 IU vitamin D3 daily for 3 years (and they took calcium supplements if dietary intake was < 1,200 mg calcium/day).
Results: The incidence of hypercalcemia varied between the vitamin D groups, ranging from 0 in the 400 IU group, to 3% and 9% in the 4,000 and 10,000 IU groups, respectively (P < .001) and the incidence of hypercalciuria was 17% in the 400IU group, 22% and 31% in the 4,000IU and 10,000 IU groups, respectively (P = .04). (When there was hypercalciuria, it was resolved by reducing calcium intakes/stopping supplements.) Of note, the researchers also refer to a dose-related negative effect on bone microarchitecture in one abstract (1). The researchers recommend “… that clinicians and patients consider [these findings] when weighing the risks and benefits of highdose vitamin D supplementation" (2), which makes me curious to read the full results when they are published!
The VITAL study at Harvard U in Boston, USA, released its long-awaited results in November 2018 as well (3,4). This randomized, placebo-controlled trial provided vitamin D3 at a dose of 2000 IU per day and marine n−3 fatty acids at a dose of 1 g per day (together and separately) to men 50 years of age or older and women 55 years of age or older in the United States. The primary end points tracked were major cardiovascular events (myocardial infarction, stroke, or death from cardiovascular causes) and invasive cancer of any type, to study primary prevention of these outcomes.
Results: “Supplementation with n−3 fatty acids did not result in a lower incidence of major cardiovascular events or cancer than placebo.”(3) and “ Supplementation with vitamin D did not result in a lower incidence of invasive cancer or cardiovascular events than placebo.” (4).
So, what are the recommendations out there?
In the United States, the recent Position of the Academy of Nutrition and Dietetics on Micronutrient Supplementation discusses the effect of nutrient supplementation on chronic disease prevention (5). With respect to vitamin D, the Academy cites recent recommendations of the US Preventive Services Task Force (USPSTF). In 2018, the USPSTF recommended against daily supplementation of 400 IU or less of vitamin D and 1,000 mg or less of calcium for the primary prevention of fractures in postmenopausal women, and further concluded there wasn’t enough evidence to recommend any dose for fracture prevention among community-dwelling men and premenopausal women (6).
In Ireland, researchers reviewed data from a hospital laboratory, evaluating trends in serum 25-hydroxyvitamin D (25OHD) levels between 1993 and 2016 (7). They observed that the yearly increase in mean 25OHD over the past 24 years was approximately 1 nmol/L/year and continuing to rise, likely due to higher oral intakes of vitamin D. Their concluding dual concern is that “policies to prevent hypovitaminosis D must be offset by strategies to avert hypervitaminosis D” (7).
In Canada, Health Canada continues to explore regulatory options for “supplemented foods” (foods containing high levels of added nutrients) and non-prescription natural health products (NHPs - soon to be called “self-care products”, including vitamins and minerals). There is even some pressure to allow an increased dose of vitamin D to be sold in Canada. Health Canada is currently exploring whether to allow vitamin D supplements to become available in doses of 2000 IU/dose – there will be public consultation in early 2019 on this issue.
So what have I decided? Well, since I had already bought some vitamin D tabs, I’ll just finish these 1000 IU tablets by taking them every other day this winter – a little won’t hurt even if it doesn’t help, but a lot is not recommended! And I won’t take any extra calcium or fish oil, since my dietary intake is pretty good – there doesn’t appear to be any extra value for primary prevention of chronic diseases.
Writing about these ‘surprising findings’ reminds me of one of our ‘brand’ positioning lines: “Dietitians are driven by curiosity to understand the science behind food and its connection to health.” (https://www.dietitians.ca/Member/Get-Involved/Dietitian-Brand-Initiative/Positioning-Lines.aspx) Yes – we are always curious, and sometimes surprised!
Written by:
Pat Vanderkooy, MSc, RD
Manager, Public Affairs – Food & Nutrition
References
- 400, 4,000 or 10,000 IU Vitamin D Daily for 3 Years: Dose-Related Negative Effect on Bone Microarchitecture” (Hanley D et al, Cdn J Diabetes 42(5):S2, 2018. Abstract available from: https://doi.org/10.1016/j.jcjd.2018.08.005
- American Society for Bone and Mineral Research Annual Meeting News: Vitamin D supplementation associated with dose-response increase in hypercalciuria. Available from: https://www.healio.com/endocrinology/reproduction-androgen-disorders/news/online/%7Bc60e8ffe-464b-4c07-819b-02e3e7428b80%7D/vitamin-d-supplementation-associated-with-dose-response-increase-in-hypercalciuria
- Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, Gibson H, Albert CM, Gordon D, Copeland T, D'Agostino D, Friedenberg G, Ridge C, Bubes V, Giovannucci EL, Willett WC, Buring JE; VITAL Research Group. Marine n-3 Fatty Acids and Prevention of Cardiovascular Disease and Cancer. N Engl J Med. 2018 Nov 10. [Epub ahead of print] Available from: https://www.ncbi.nlm.nih.gov/pubmed/30415637
- Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, Gibson H, Gordon D, Copeland T, D'Agostino D, Friedenberg G, Ridge C, Bubes V, Giovannucci EL, Willett WC, Buring JE; VITAL Research Group. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Engl J Med. 2018 Nov 10. [Epub ahead of print] Available from: https://www.ncbi.nlm.nih.gov/pubmed/30415629
- Ventura Marra M, Bailey RL. Position of the Academy of Nutrition and Dietetics: Micronutrient Supplementation. J Acad Nutr Diet 118(11): 2162–2173. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/30366569
- Final Update Summary: Vitamin D, Calcium, or Combined Supplementation for the Primary Prevention of Fractures in Community-Dwelling Adults: Preventive Medication. U.S. Preventive Services Task Force. April 2018. Available from:
https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/vitamin-d-calcium-or-combined-supplementation-for-the-primary-prevention-of-fractures-in-adults-preventive-medication
- McKenna MJ, Murray B, Crowley RK, Twomey PJ, Kilbane MT. Laboratory trend in vitamin D status in Ireland: Dual concerns about low and high 25OHD. J Steroid Biochem Mol Biol. 2018 Oct 5. doi: 10.1016/j.jsbmb.2018.10.001. [Epub ahead of print] Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/30296586
PEN System is definitely “making the GRADE”
I was surprised (and pleased) to see that PEN now contains evidence-based recommendations for 18 practice questions  developed using the GRADE approach. As we’ve shared previously, the GRADE method is considered the gold standard for critical appraisal and guideline development. Here are the PEN GRADE questions:
developed using the GRADE approach. As we’ve shared previously, the GRADE method is considered the gold standard for critical appraisal and guideline development. Here are the PEN GRADE questions:
Thanks to all our PEN authors and reviewers for making this content possible.
Written by:
Jayne Thirsk RD, PhD, FDC
Senior Director, Knowledge Translation
Time Flies
In an email note last month to colleagues I mentioned that I was finding that time was going by faster  and asked if someone might help slow it down! While a monthly task was sent around a week earlier than usual which helped to prompt this feeling, I did think that once my kids had left home that time would slow down a bit.
and asked if someone might help slow it down! While a monthly task was sent around a week earlier than usual which helped to prompt this feeling, I did think that once my kids had left home that time would slow down a bit.
Looking briefly at the literature it seems the study of time passage has been ‘a thing’ for some time. Lewis writes in her Scientific American post (1) that psychologist William James noted in 1890 that as we age, time seems to speed up.
So why is this?
William James hypothesized that it is because as adults we don’t have as many memorable events as we would have had when were younger (1,2). Stress, or the pressure of perceived time appears to play a big part as well (1,3).
What doesn’t appear clear is if the passage of time is perceived to be faster only by older adults (3). Friedman and Janssen (4) studied reports from 1865 individuals (16-80 years) and found no clear differences of how the passage of time perception changes with aging. Another study assessing the ‘direct experience of the flow of time in everyday life’ in 15 younger adults and 14 older adults measured through experience sampling methodology (ESM) questionnaires, completed at different times throughout the day, showed that both age groups felt that time passed more quickly as they aged and that time passes faster in the present than when they were younger (5). This was significantly related to emotional states and the how much an activity captivated their attention.
This research on the perception of time as we age is interesting, and more is needed related to emotional factors and the activities that capture attention to better understand perceived time passage between the ages (3). In reality though, “time is not literally getting faster” (1) and likely what is most important is to not dwell on time but instead on enjoying the activities you are involved with.
Written by:
Jane Bellman, MEd, RD
Online Education and PEN Resource Manager, Dietitians of Canada
References
- Lewis JG. Why does time fly as we get older? MIND Guest Blog. Scientific American. December 18, 2013. Available from: https://blogs.scientificamerican.com/mind-guest-blog/why-does-time-fly-as-we-get-older/
- James, W. The Principles of Psychology (2 vols.). New York: Henry Holt; 1890.
- Di Crosta A, La Malva P. Commentary: Experience Sampling Methodology reveals similarities in the experience of passage of time in young and elderly adults. Front Psychol. 2017 Aug;8:1384. doi: 10.3389/fpsyg.2017.01384. eCollection 2017. Citation available from: https://www.ncbi.nlm.nih.gov/pubmed/28848486
- Friedman WJ, Janssen SMJ. Aging and the speed of time. Acta Psychol (Amst). 2010 Jun;134(2): 130-41. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/20163781
- Droit-Volet S, Wearden JH. Experience Sampling Methodology reveals similarities in the experience of passage of time in young and elderly adults. Acta Psychol (Amst). 2015 Mar;156:77–82. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/25701720
Calcium Supplementation and PMS
I was surprised at the strength of evidence (Grade B) of taking calcium supplements (but not other supplements) for reducing premen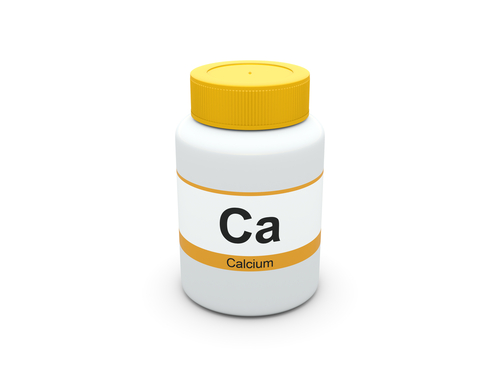 strual menstrual syndrome symptoms. Supplementation of 1000-1200 mg/day of calcium carbonate resulted in a 50% reduction of symptoms (depression, tension, mood swings, crying spells, anxiety) as reported in a systematic review. Women should be advised to not exceed the upper tolerable maximum limit of 2000-2500mg of elemental calcium from all sources. For more information see PEN® Practice Question: Do dietary supplements reduce the symptoms of premenstrual syndrome (PMS)?
strual menstrual syndrome symptoms. Supplementation of 1000-1200 mg/day of calcium carbonate resulted in a 50% reduction of symptoms (depression, tension, mood swings, crying spells, anxiety) as reported in a systematic review. Women should be advised to not exceed the upper tolerable maximum limit of 2000-2500mg of elemental calcium from all sources. For more information see PEN® Practice Question: Do dietary supplements reduce the symptoms of premenstrual syndrome (PMS)?
Written by:
Kerri Staden, BSc, RD
PEN® Resource Manager
Using levies to improve eating behaviours
In the SACN report from 2015 (1), they recommended that ‘free sugars’ (added to foods and drinks, found in honey,  syrups and fruit juice) should provide no more than 5% of total daily energy intake. Reports from the UK National Diet and Nutrition Survey (NDNS) from 2014-2016 (published in 2018) suggest that sugar makes up 13.5-14.1% of children aged 4-18yrs daily calories intake with sugary drinks being the main source of sugar for teenagers (2).
syrups and fruit juice) should provide no more than 5% of total daily energy intake. Reports from the UK National Diet and Nutrition Survey (NDNS) from 2014-2016 (published in 2018) suggest that sugar makes up 13.5-14.1% of children aged 4-18yrs daily calories intake with sugary drinks being the main source of sugar for teenagers (2).
I welcomed the UK government’s Soft Drinks Industry Levy being introduced in April this year as a step to helping to reduce childhood obesity. The BDA supported this levy and produced a policy statement following this.
The Levy is charged at two rates; 24p/litre on drinks with more than 8g added sugar per 100ml and 18p/litre for drinks between 5 and 8g per 100ml.
The soft drinks industry has been reducing sugar and calories intake on soft drinks since 2013, this is down to 16.8% from 18.7% in 2013 according to the British Soft Drinks Association (3).
The PEN System’s knowledge pathway on child and youth nutrition provides an evidenced-based recommendation on interventions to help reduce the consumption of energy from sugar-sweetened beverages (SSBs) in children. Limiting the availability of SSB in schools and developing education programmes aimed at reducing the intake of SSB are two interventions supported by RCT.
It will be interesting to see the results from the next NDNS to see if the levy as well as other interventions (such as those recommended by PEN) further reduce the intake of sugar. The levy is a positive step at tackling childhood obesity, but the complex issue clearly requires many more steps from the government and industry.
I was surprised to find a research study using a coupled modelling framework on optimal taxation for red and processed meat consumption following the sugar levy (4). With an estimated average taxation of 25%, the study estimated that the consumption of processed meat would decrease by 16% whilst red meat remained the same. The study reported that the estimated number of deaths related to the consumption from red and processed meat would decrease by 9%. As this study used a modelling framework, the findings rely on many assumptions which may not be replicated in real life. The study is also unable to control for confounding factors and consider what the meat intake may be replaced with. Unlike free sugars, there are nutritional qualities of meat which would also be an important factor to consider.
Written by:
Eleanor Johnstone PG Dip, BSc, RD
Policy Officer (Education & Professional Development)
References:
- Public Health England. SACN Carbohydrates and Health Report. (2015). Available from: https://www.gov.uk/government/publications/sacn-carbohydrates-and-health-report
- Public Health England. National Diet and Nutrition Survey. (2018) Available from: https://www.gov.uk/government/statistics/ndns-results-from-years-7-and-8-combined
- The British Soft Drinks Association. Position Statement. (no date). Available from: http://www.britishsoftdrinks.com/Position-Statements/soft-drinks-tax
- Springmann M, Mason-D’Croz D, Robinson S, Wiebe K, Godfray HCJ, Rayner M, et al. Health-motivated taxes on red and processed meat: A modelling study on optimal tax levels and associated health impacts. (2018) 13 (11). Available from: https://doi.org/10.1371/journal.pone.0204139
Primary and Secondary CVD Prevention and Daily Fish Intake – Wow!
As the Editor for PEN, I review all of the content that is published on the website. I have to confess there are not many  items that catch me off guard, as I am always expecting change due to the nature of our profession and the volume of research that is continually published.
items that catch me off guard, as I am always expecting change due to the nature of our profession and the volume of research that is continually published.
The recent update to the practice question on omega-3 fatty acids on primary and secondary prevention of cardiovascular disease really surprised me. This GRADE practice question includes the following recommendations:
The focus on obtaining omega-3 fatty acids through food and not supplements does not surprise me, nor does the risk-decreasing potential of eating fish. Although I don’t always remember what I edit, I do remember the overall themes. One of which is that in many cases nutrients obtained via food are better utilized in the body that nutrients obtained via supplements.
What surprised me was the recommendation for daily fish intake. I understood why the recommendation was made as it is supported by evidence (albeit low quality evidence from observational studies), but daily fish intake? How does that work and what are the individual/family, environmental and economic implications? On an individual level, I have been trying to incorporate fish into my diet (and my husband’s!) on a daily basis. Living in Newfoundland and Labrador, fish availability is not a challenge and canned salmon is always easy. I haven’t been able to consume fish seven days a week yet, but I am hoping 6 oz on one day counts for two! My children are now young men, but what if they were still sitting at my table every day for their meals? Would daily fish be acceptable to them?
What about on environmental and economic levels? Is the impact of additional fish consumption balanced by the decrease in other animal protein sources? What about fish stocks? Does this impact on the long-term viability of fish stocks and/or does it create opportunity for enhanced markets and businesses? It is fascinating to consider the many impacts that one recommendation can potentially have. It is also important to consider that this one recommendation needs to be considered in the context of overall heart healthy dietary patterns that promote vegetables, fruit, whole grains, legumes and nuts, and limit sources of free sugars, saturated fat and trans fat.
See Additional Content:
Written by:
Heather Alaverdy MA, RD
PEN Editor
Surprising findings about Fluoride
As I am working on a PEN GRADE review of the evidence about the health effects of fluoride, I have learned 2 surprising findings:
- Some of the health concerns are real when the fluoride dose is high enough, and
- the studies that support fears about fluoride often have design flaws and are frequently misreported.
It is all about the dose
In Canada, Australia and other countries where fluoride is added to water supplies, it is added at 0.7 mg/L (1,2). The amount was decreased from 1 mg/L a few decades ago to .jpg) optimize the dental benefits in terms of less decayed missing and filled teeth, while minimizing the appearance of dental fluorosis. Mild dental fluorosis appears as some whiter spots on the teeth while severe fluorosis can appear as yellow to brown staining and create uneven surfaces.
optimize the dental benefits in terms of less decayed missing and filled teeth, while minimizing the appearance of dental fluorosis. Mild dental fluorosis appears as some whiter spots on the teeth while severe fluorosis can appear as yellow to brown staining and create uneven surfaces.
Some communities with very high fluoride concentrations in the water supplies such as 15 mg/L (3,4) have provided a natural experiment to examine health effects of higher levels of fluoride, and how fluoride concentrations are related to fluorosis. Most of the areas that have very high fluoride concentrations in the water supplies are in the middle east countries (5) and some communities in Mexico (3).
Some individuals in a population are likely to have high intakes of fluoride independent of water fluoridation levels. People who drink large quantities of strong tea (6) and young children who swallow fluoridated toothpaste (7) can have higher than desirable fluoride intakes from these sources. The Tolerable Upper Intake Level for Fl is 10 mg/d. (8,9)
Examples of studies that are used to support fears about fluoride:
- A mouse study with 97 times the recommended dosing: 68 mg/L instead of 0.7 mg/L (10).
- A study referred to as “Impact of drinking water fluoride on human thyroid hormones: A case-control study) mis-reports their null findings and used very unusual analysis and reporting methods (11). The only analysis that used the study’s case-control design appropriately was not reported accurately. Their study found no risks of fluoride in drinking water but they concluded that “standard household water purification devices was recommended for hypothyroidism”. This concluding statement suggests some risk when no risk was identified.
- A more recent study reported an association between urinary fluoride in pregnancy and parental reported symptoms of ADHD and inattention in the offspring in Mexico City (12). These researchers did not measure the water fluoride content but did note in their introduction that some of the water has contents that ranged up to 1.4 mg/L (twice the usual water fluoridation level) and that fluoride was also added to salt as a supplemental source. Since the water in Mexico City naturally contains fluoride at levels higher than usual fluoridation levels, these researchers should have measured the water and mentioned this data in their paper to be able to provide context to their findings.
In summary, after in-depth reading about health effects of fluoride, I have learned that fluoride in very high doses can be of a concern, particularly to the appearance of teeth and perhaps some other health effects, but the dose is key. The analyses and write ups of studies that suggest that fluoride is of higher risks has generally been poorly conducted and subject to biased reporting of results. Unfortunately, this biased reporting may contribute to an inaccurate picture of the evidence. I encourage everyone to look at the fluoride doses people are exposed to in the studies and to pay attention to the analysis methods used in the studies. Everything, including water and oxygen, are toxic in extremely high doses. Health effects of any substance at extremely high doses do not inform us about the health effects at carefully controlled doses.
Written by:
Tanis Fenton PhD RD FDC
Dietitian/Nutritionist, Epidemiologist,
PEN® Evidence Analyst, Associate Professor, University of Calgary
References
- Jack, B., Ayson, M., Lewis, S., Irving, A., Agresta, B., Ko, H., Stoklosa, A. 2016, Health Effects of Water Fluoridation: Evidence Evaluation Report, report to the National Health and Medical Research Council, Canberra. Available from: http://fluoridealert.org/wp-content/uploads/nhmrc.evidence-report.final_.8-24-16.pdf
- The State of Community Water Fluoridation across Canada. 2017 Available from: https://www.canada.ca/en/services/health/publications/healthy-living/community-water-fluoridation-across-canada-2017.html
- González-Horta C, Ballinas-Casarrubias L, Sánchez-Ramírez B, Ishida MC,Barrera-Hernández A, Gutiérrez-Torres D, et al. A concurrent exposure to arsenic and fluoride from drinking water in Chihuahua, Mexico. Int J Environ Res Public Health. 2015 Apr 24;12(5):4587-601. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4454927/
- Rango T, Vengosh A, Jeuland M, Whitford GM, Tekle-Haimanot R. Biomarkers of chronic fluoride exposure in groundwater in a highly exposed population. Sci Total Environ. 2017 Oct 15;596-597:1-11. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5528157/
- Water sanitation hygiene. World Health Organization. http://www.who.int/water_sanitation_health/diseases-risks/diseases/fluorosis/en/. Accessed: Nov 29, 2018
- Das S, de Oliveira LM, da Silva E, Liu Y, Ma LQ. Fluoride concentrations in traditional and herbal teas: Health risk assessment. Environ Pollut. 2017 Dec;231(Pt 1):779-784. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/?term=28865383
- Bentley EM, Ellwood RP, Davies RM. Fluoride ingestion from toothpaste by young children. Br Dent J. 1999 May 8;186(9):460-2. Abstract available at: https://www.ncbi.nlm.nih.gov/pubmed/?term=10365494
- Dietary Reference Intakes: The essential guide to nutrient requirements. 2006. Fluoride. The National Academies Press. https://www.nap.edu/read/11537/chapter/35 Accessed Nov 29,2018
- Nutrient Reference Values for Australia and New Zealand: Fluoride 2017. Australian Government/National Health and Medical Research Council. https://www.nrv.gov.au/nutrients/fluoride Accessed Nov 29,2018
- Li X, Zhang J, Niu R, Manthari RK, Yang K, Wang J. Effect of fluoride exposure on anxiety- and depression-like behavior in mouse. Chemosphere. 2019 Jan;215:454-460. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/?term=30336322
- Kheradpisheh Z, Mirzaei M, Mahvi AH, Mokhtari M, Azizi R, Fallahzadeh H,Ehrampoush MH. Impact of Drinking Water Fluoride on Human Thyroid Hormones: A Case-Control Study. Sci Rep. 2018 Feb 8;8(1):2674. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5805681/
- Bashash M, Marchand M, Hu H, Till C, Martinez-Mier EA, Sanchez BN, Basu N,Peterson KE, Green R, Schnaas L, Mercado-García A, Hernández-Avila M, Téllez-Rojo MM. Prenatal fluoride exposure and attention deficit hyperactivity disorder (ADHD) symptoms in children at 6-12 years of age in Mexico City. Environ Int. 2018 Dec;121(Pt 1):658-666. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/?term=30316181
Nutritional considerations for transgender people
While recently the focus for the PEN team has been updating older content we do like to look ahead to see what new  topics we should be adding. In doing so, I came up with the topic of transgender people and wondered about any particular nutritional requirements or health issues.
topics we should be adding. In doing so, I came up with the topic of transgender people and wondered about any particular nutritional requirements or health issues.
The article by Fergusson P, Greenspan N, Maitland L and Huberdeau R: Towards Providing Culturally Aware Nutritional Care for Transgender People: Key Issues and Considerations is a key one for all dietitians to read whether you work specifically with this population or not. As the authors indicate, dietitians, “need to be aware of key issues in transgender health to provide culturally competent clinical nutritional care” (1). In addition to learning about the terminology of gender identity and that the terms are constantly evolving, the article makes recommendations for providing safe health and nutritional care. As a topic new to me, most of the article could be classified as “surprise findings” such as which equation to use to calculate energy requirements, establishing healthy weight because of changing muscle mass, etc. Perhaps the greatest surprise to me, because I hadn’t thought of the implications, was the possible increased risk of cardiovascular disease because of oral ethinyl estradiol – a hormone prescribed for male to female transgender people. This issue of increased risk of CVD is further explained in an article by Gooren et al who indicates that people with pre-existing cardiovascular risk should probably be prescribed transdermal estrogens (2).
Reading this article led me to wonder what is being taught these days in the university nutrition / dietetic programs. I assume and hope that the topic is being addressed. Dietitians need to be ready to be “trans-friendly and respectful” in their practice (3).
Written by:
Beth Armour, MEd, P.Dt
PEN® Content Manager
Dietitians of Canada
References:
- Fergusson P, Greenspan N, Maitland L, Huberdeau R. Towards Providing Culturally Aware Nutritional Care for Transgender People: Key Issues and Considerations. Can J Diet Pract Res. 2018 Jun 1;79(2):74-79. doi: 10.3148/cjdpr-2018-001. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/29543495
- Gooren LJ, Wierckx K, Giltay EJ. Cardiovascular disease in transsexual persons treated with cross-sex hormones: reversal of the traditional sex difference in cardiovascular disease pattern. Eur J Endocrinol. 2014 Jun;170(6):809-19. doi: 10.1530/EJE-14-0011. Abstract available from: https://www.ncbi.nlm.nih.gov/pubmed/24616414
- Morley C, Morley R. Toward trans-friendly and respectful dietetic practice. Can J Diet Pract Res. 2017;78(3):162–3. Research abstract available from: http://dcjournal.ca/doi/pdfplus/10.3148/cjdpr-2017-024